Sleep
- Dr. Thomas J. Lewis

- Mar 3, 2024
- 8 min read
Lack of quality sleep is the #3 complaint I hear behind, lack of energy, and chronic pain.
Lack of sleep drives at least 1 of 5 disease mechanisms: "thrive vs survive." When you lack sleep, your brain and eyes suffer the most. Why? They are the most metabolically active and do not take a break until you sleep. I explain this as follows. You do NOT repair your car engine while it is running.
When I'm sleep-deprived, my mental functioning is similar to that of someone with dementia. After a poor night's sleep, I often stumble aimlessly and am much more likely to spill my water or coffee as I try to "pull it together."
One of our webinar regulars, a highly intelligent and informed individual, overnighted at a Scalar energy center. Another attendee "snored loudly all night long." I asked Steve his impression of the Scalar experience. This is what he said.
"I don't know because none of us slept, and the group was collectively miserable the next morning."
Conclusion: A good night's sleep is much more beneficial than a Scalar Energy session!
Here is an example of advice we give people with sleep complaints. Sadly, I think this touches the surface of the underlying issues. That's why anyone with sleep problems should schedule sessions with Dr. Michelle Gamble (found on our home page). Regardless, some of these suggestions may help with physiological issues, not emotional ones.
Sleep is mainly a time for your brain and eyes to recover and repair from their day-long efforts. Is your bicep exhausted just before bed? Probably not. But if you were doing arm curls all day long, it certainly would be. Your brain is tired since it has been active all day long. Our brains are energy hogs. 25% of the blood leaving our heart pumps through our brain, yet our brains are small compared to the rest of our body - being only about 2.5% of our mass. Thus, the brain sees 10 times the blood flow.
During sleep, the brain progresses through alternating cycles of light and deep sleep – or sleep stages. These alternating sleep stages allow the brain to heal and restore itself. Sleep problems can cause issues with memory, thinking, mood (depression, anxiety), and chronic fatigue/chronic pain. During sleep, the brain can repair and grow cells, tissue, and nerves that regenerate and boost the hormones and immune system. Along with good nutrition and stress reduction, restorative sleep is vital for optimal physical, mental, and emotional health.
The best supplements for good sleep are:
• Probiotics and prebiotics: The gut's "enteric nervous system" produces "happy" hormones and neurotransmitters. Optimal gut health ensures micronutrient availability for your energetic brain.
• Cod liver oil: Fish oils and fat-soluble nutrients found in cod liver oil are key brain and eye repair components. They are also anti-inflammatory.
• Melatonin: Melatonin is very effective in helping induce and maintain sleep in children and adults. It is most apparent in improving sleep when melatonin levels are low. Melatonin supplementation is most helpful in improving sleep quality in people 40 and older, as it is more common to find low melatonin levels in this age group. Since your body produces melatonin, avoid taking it daily. Take it occasionally instead, and keep a journal to determine if it is effective for you.
Test for and treat infections that may be activating your brain immune cells (microglial cells)
• The amino acid glycine, taken before bedtime, helps the body reach deep sleep more quickly. It also helps raise the surface temperature of the feet and reduce the core body's temperature. People wake up feeling refreshed, without the drowsiness some sleep remedies can cause. Glycine is produced naturally and in many healthy foods, including fish, meat, and beans.
• GLYCINE EVIDENCE & DOSE: Abstract In human volunteers who have been continuously experiencing unsatisfactory sleep, effects of glycine ingestion (3 g) before bedtime on subjective sleep quality were investigated, and changes in polysomnography (PSG) during sleep were analyzed. Effects on daytime sleepiness and daytime cognitive function were also evaluated. Glycine improved subjective sleep quality and sleep efficacy (sleep time/in-bed time) and shortened PSG latency to sleep onset and slow wave sleep without changes in the sleep architecture. Glycine lessened daytime sleepiness and improved the performance of memory recognition tasks. Thus, bolus ingestion of glycine before bedtime produces subjective and objective sleep quality improvement differently than traditional hypnotic drugs such as benzodiazepines.
ARTICLE TITLE: Glycine ingestion improves subjective sleep quality in human volunteers, correlating with polysomnographic changes
• Dr. Michael Murray, N.D. has some additional suggestions at this site:
Here is a link to several videos we assembled on improving sleep.
Test for and treat infections that may be activating your brain immune cells (microglial cells)
Here I dive into how inflammatory organisms can impact sleep and visa versa.
ABSTRACT:
Sleep is considered an important modulator of the immune response. Thus, a lack of sleep can weaken immunity, increasing organism susceptibility to infection.
For instance, shorter sleep durations are associated with a rise in suffering from the common cold.
The function of sleep in altering immune responses must be determined to understand how sleep deprivation increases the susceptibility to viral, bacterial, and parasitic infections.
There are several explanations for greater susceptibility to infections after reduced sleep, such as impaired mitogenic proliferation of lymphocytes, decreased HLA-DR expression, the upregulation of CD14+, and variations in CD4+ and CD8+ T lymphocytes, which have been observed during partial sleep deprivation.
Also, steroid hormones, in addition to regulating sexual behavior, influence sleep. Thus, we hypothesize that sleep and the immune-endocrine system have a bidirectional relationship in governing various physiological processes, including infection immunity.
This review discusses the evidence on the bidirectional effects of the immune response against viral, bacterial, and parasitic infections on sleep patterns and how the lack of sleep affects the immune response against such agents.
Because sleep is essential in maintaining homeostasis, these situations must be adapted to elicit changes in sleep patterns and other physiological parameters during the immune response to infections to which the organism is continuously exposed.
FROM THE BODY OF THE PAPER
Many studies have demonstrated that total sleep deprivation and rapid eye movement (REM) sleep deprivation modify various components of the immune system, such as the percentage of cell subpopulations (e.g., CD4+, CD8+, and NK) and cytokine levels (e.g., IFN-g, TNF-a, and IL-1) [3–5].
Also, conversely, sleep patterns are altered during the immune response, suggesting that sleep and the immune response are linked through bidirectional communication.
During sleep, important processes occur concerning endocrine function in mammals, such as rises in the levels of hormones such as prolactin and growth hormone [10]. On the contrary, cortisol levels decline, peaking before one wakes up [10, 11], demonstrating a connection between sleep and other physiological events.
THIS NEXT CONCEPT IS EXTREMELY IMPORTANT - IMMUNITY ONLY FIGHTS INFECTIOUS SPECIES - IT GOES UP OR DOWN FOR NO OTHER REASON.
Innate immunity is the first line of defense. Its two primary functions are
to isolate and destroy invading pathogens through inflammatory processes and
to recognize and process antigens to affect acquired immunity. Both types of immunity include cellular and biochemical mechanisms that are designed to respond quickly to infections and accurately distinguish between native and foreign materials.
The brain is linked to the immune system, and similar interactions occur during sleep, wherein brain activity changes, resulting in the putative “awake brain” and “sleeping brain.” There is evidence that the expression of molecules, such as neurotransmitters, hormones, and cytokines, is modulated while the subject sleeps, and human studies have described changes in the serum levels of some of these components during sleep. Specifically, secretion of IL-1β, IL-10, IL-12, and TNF-α by monocytes and dendritic cells peaks during sleep, independently of circadian rhythms.
This behavior may be directly related to sleep because when the animal is deprived of the rhythmicity of these cytokines [26, 27], the changes in expression wane. Also, blood levels of monocytes, T cells, and NK cells follow a clear circadian rhythm regarding the sleep-wake cycle [3].
*** IMPORTANT: Cortisol and melatonin are not the only physiological substances that change during waking and sleeping cycles.****
This evidence implicates an interaction between components of the immune system and the mechanisms that generate sleep. Thus, the changes that occur during sleep when an immune response is mounted against a pathogen should be described.
Several infectious diseases are associated with sleep disorders. Particularly, infectious agents, such as viruses, bacteria, and parasites, infect the CNS and cause sleep disorders, due to the immune response that is generated against the infection or through direct effects by the pathogen. Moreover, other invasive agents that cause sleep disturbances affect other systems, such as the respiratory and endocrine systems—not those that regulate sleep.
Viruses cause many diseases, including pandemics, such as influenza and immunodeficiency virus (HIV). These diseases present with a variety of symptoms, depending on the organ and system that is infected, but many of these conditions are accompanied by sleep disturbances, fatigue, and fever. For example, intranasal inoculation with influenza virus in mice enhances non-rapid eye movement sleep (NREM) and decreases rapid eye movement sleep (REM), despite body temperature declining [39–42].
Bacteria are another large group of pathogens that infect and cause disease, significantly altering the body's overall functioning. A study in which humans were inoculated with Salmonella abortus endotoxin reported significant declines in waking and REM sleep, accompanied by greater non-REM sleep [77]. In contrast to the changes in experimental animals, this endotoxin did not increase the amplitude of delta waves [77]. A subsequent study demonstrated that Salmonella abortus endotoxin reduced the total duration of NREM sleep, whereas waking, sleep latency, and daytime sleepiness increased [78].
Parasitic infections can also alter sleep patterns due to the resulting immune response or through direct effects. Because parasites are multicellular organisms, they can modify certain behaviors to facilitate infection and complete their life cycle [89]. Sleep may be a state in which they can exploit the infected host because the responsiveness to external stimuli declines, rendering the host more susceptible to infection. However, there is little evidence of this relationship.
SELECTED CONCLUSIONS - Consider reading this long paper.
In recent decades, much experimental and clinical evidence has been generated on the existence of and interaction between the neuroendocrine and immune systems. This communication network allows the body to maintain homeostasis, particularly when responding to a stimulus, such as an infection. The body must alter its metabolic functions during an infection to eliminate the pathogen. For example, it must devote most of its energy to the immune system, leaving the remainder of the body with less input.
We are merely beginning to understand how infections change sleep patterns, and why sleep is altered during illness remains unknown. One hypothesis suggests that altered sleep during infection is a component of the acute phase response, promoting recovery during illness, likely through mechanisms that involve cytokines and their receptors, as well as receptors of the innate immune system.
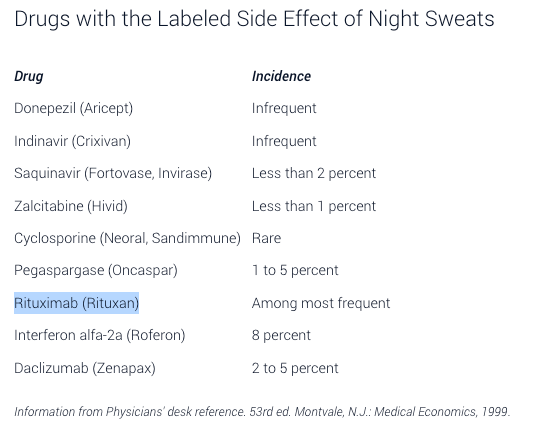
Not mentioned in the article is night sweats.
From Mayo Clinic
Night sweats can be related to infection. For example, if you've recently been ill with a minor respiratory infection, a slight fever can cause you to sweat more at night, as your body's normal day/night temperature reset may be exaggerated.
More serious infections that can cause night sweats include tuberculosis or other bacterial infections, fungal diseases and unusual and more chronic conditions, such as disorders of the nervous system or in the body's hormone-producing glands (endocrine system). Occasionally, diseases such as cancer cause temperature elevations and night sweats.
So if the night sweats are a new symptom, particularly if they are associated with red flags such as fever, change in appetite — particularly decrease in appetite — weight loss, lymph node swelling or rash, you should see a physician for evaluation.
Amy!
Weekly Webinar Links: Join us for detailed health information - at no charge. All are welcome.
Monday at noon EST -
Wednesday at 8 pm EST -

Be Bold - Be Brave - Stay Well












Comments